School is back in session, Halloween decorations are already picked through at Joann’s, and the evenings are getting cooler. Fall is here! And that means we should start thinking about getting our fall vaccines.
Why does respiratory disease peak in the fall?
Back in the day, the standard answer to this question was always that people tend to stay indoors more often in the winter and therefore would circulate more infections due to close quarters and recirculated air. As we have learned more about infectious disease, we have come to find that the answer is far more complicated than this. There is no one reason, and probably the reasons differ for different diseases and different parts of the country. But here are some of them:
Cooler, drier air. Humidity tends to decrease in the fall and winter and this changes the dynamics of sneezes and coughs. A sneeze is a complex mixture of differently sized droplets being expelled at upwards of 100MPH from the nose and mouth. The largest droplets (which tend to be the most predominant) fall to the floor and therefore are not a major source of spread.
Smaller droplets can linger in the air longer, travel further distances and therefore are more likely to get picked up by another person. Low humidity conditions evaporate more liquid from the larger droplets, making them smaller. This means that more droplets end up in the “float around” size cohort.
Reductions in immunity. The human immune system seems to be less active in the colder temperatures of winter. This can be because of less available sunlight (reducing vitamin D levels, for example), colder and drier air reduces the mucus lining in the upper respiratory tract. It’s even been discovered that immune structures in the nose that protect us from viruses are reduced in colder temperatures.
Viral structural dynamics. Many (but not all) respiratory viruses have an outer layer called an envelope. This layer is made of fats and is an essential part of the virus that allows it to attach to our cells. Fats are notoriously sensitive to things like temperature changes, salts, pH changes, soap, etc. Exposed to heat, they melt easily. So in the heat of the summer, viral envelopes may destabilize…. essentially melting off the virus. Once the virus loses its envelope, it can no longer infect us. This is not a one-size-fits-all answer though. Envelopes can also be somewhat stabilized by viral proteins. COVID-19 virus seems to be more stable than influenza at warmer temperatures, possibly due to variations in the envelope. This may at least partially explain why COVID activity seems to be more year round than flu.
What’s circulating right now?
COVID.
The three vaccine-preventable respiratory diseases that we are worrying about for fall/winter are COVID-19, Flu and Respiratory Syncytial Virus (RSV). Here are the current surveillance maps for these three diseases for the week ending on Sept. 7th.
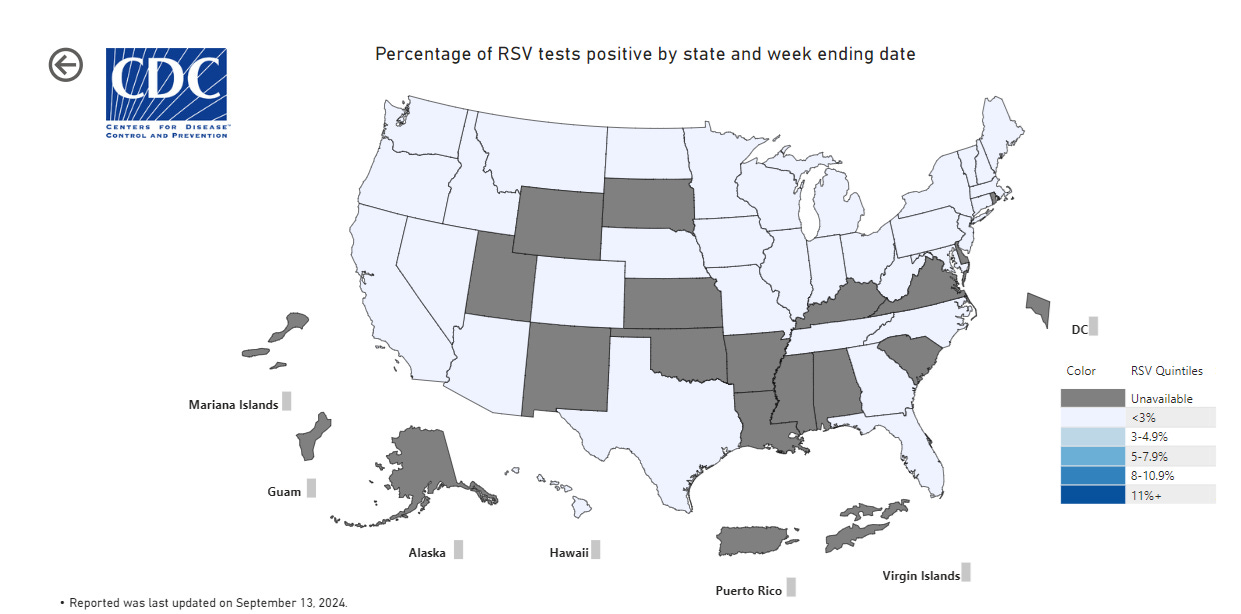
RSV:
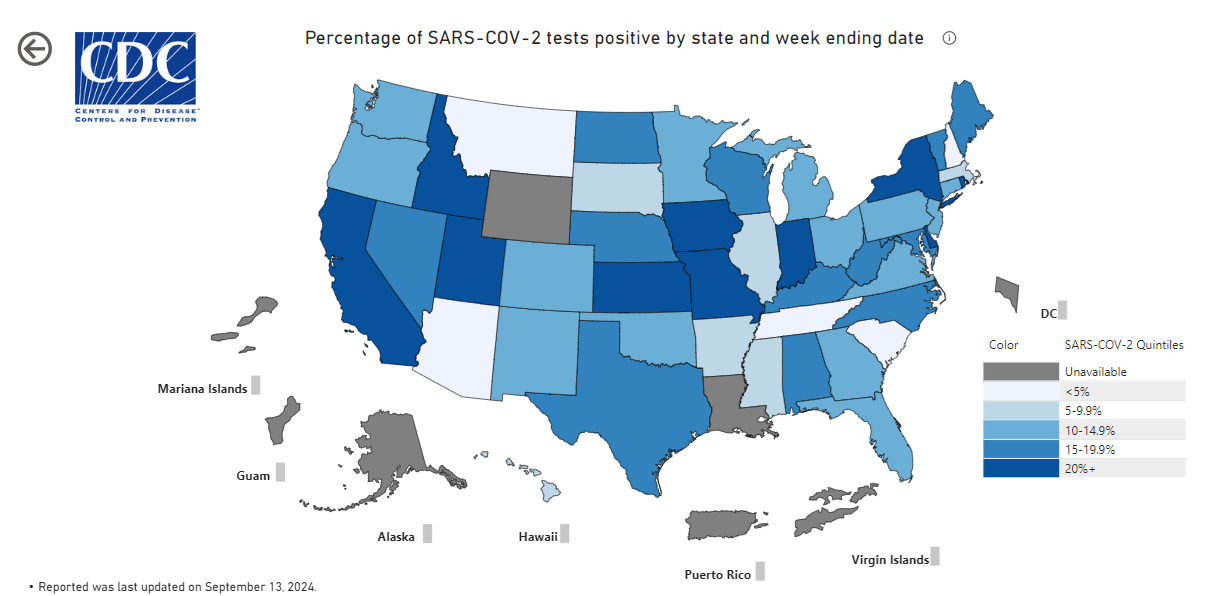
COVID-19:
Flu:
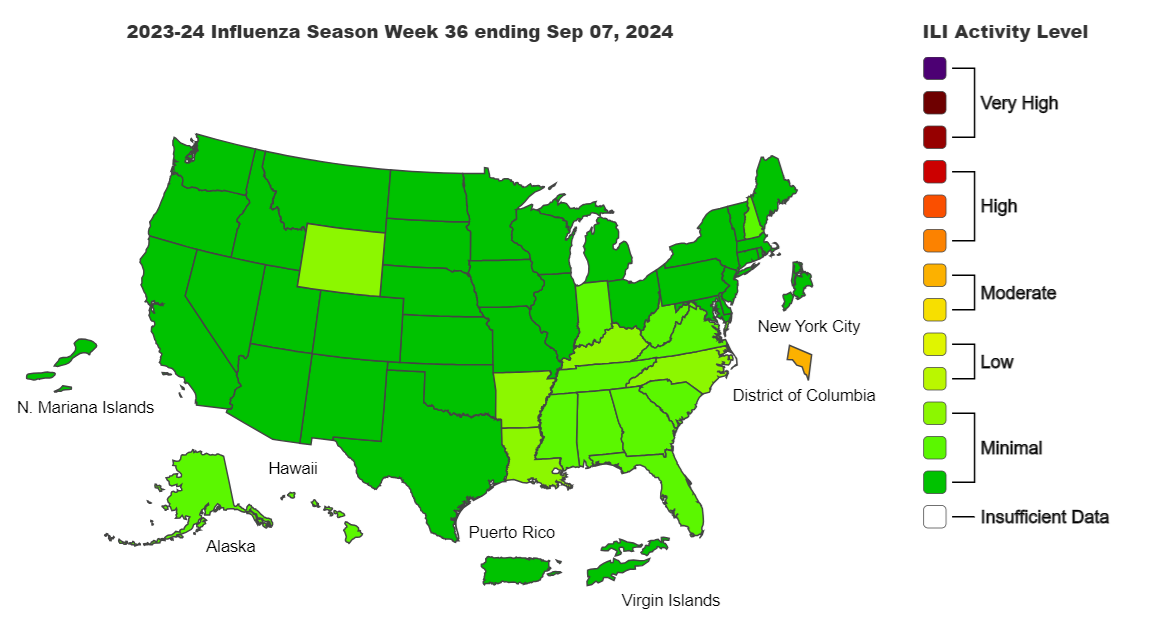
As you can see, RSV levels are very low across the USA. Flu levels are minimal to low, with the exception of Washington, DC which has entered the moderate range. But COVID-19 is circulating pretty widely (states in dark blue have the highest rates).
The CDC anticipates both Flu and RSV levels to rise as we get deeper into the fall season and are therefore recommending that Americans get COVID, Influenza and RSV vaccines. See below for the individual reccomendations.
Info about the COVID vaccines.
Everyone over the age of 6 months is recommended to get an updated COVID vaccine, especially those over age 65, those who want to prevent long-COVID, those who have predisposing conditions (see here for a comprehensive list of risk factors), live in a long-term care facility, are pregnant or breast feeding.
If you have recently been infected with COVID, you can wait 3 months before getting the updated vaccine. You should wait at least 2 months since your last COVID vaccine before getting the updated version.
Protection from the vaccine may take up to 2 weeks to develop and tends to drop off significantly after 4 months. Use that information if you are timing your COVID shot to coincide with an event, a trip or something that will increase your risk of infection/transmission. Unfortunately, COVID vaccines are no longer free for the uninsured since the CDC’s Bridge Access Program that provided free vaccines during the pandemic has ended. Updated COVID vaccines may cost up to $200 for the uninsured but there are some low- or no-cost vaccine programs available at health departments. Check here for more info.
These are the vaccines available currently, and the CDC does not recommend one over the other.
Pfizer (Comirnaty) 2024-2025: For those 6 months and over. A single dose of an mRNA vaccine for the Omicron variant KP.2
Moderna (Spikevax) 2024-2025: For those 6 months and over. A single dose of an mRNA vaccine for the Omicron variant KP.2
Novavax 2024-2025: For those 12 years and older. A single dose of a recombinant protein vaccine for the Omicron variant JN.1.
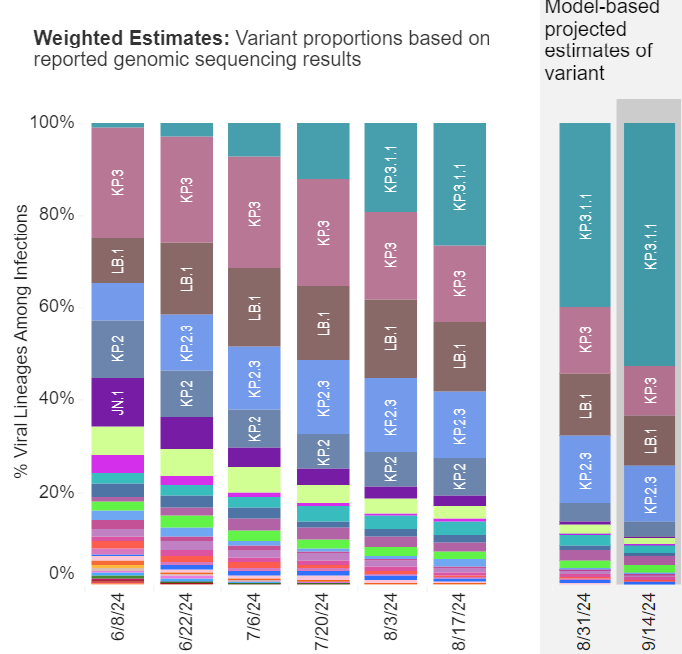
As you can see from the graph below, JN.1 (purple) is still circulating but at a much lower level than KP.2 (blue). KP.3 (pink and teal) is now the dominant strain and it is an offshoot of KP.2 with enhanced transmissibility. It is not yet known how well the 2024-2025 vaccines will protect against KP.3, but my gut feeling is that Pfizer/Moderna will provide good protection since KP.2 and KP.3 are so closely related.
Info about the Flu vaccine.
Everyone over the age of 6 months should get a flu vaccine. Those over 65 should get the high-dose flu vaccine. There are many different types of flu vaccine to choose from, consult with your pharmacist or physician for the one that is best for your particular needs (allergy, age, etc).
Since protection from the vaccine takes 2 weeks to develop and may start to wane after a few months, my favorite time to get the flu shot is in October so that I am fully protected during the holiday season when I travel and contact a lot of people. Yes, you can get the flu vaccine and the COVID vaccine at the same visit.
This year’s flu vaccine contains four strains of flu viruses:
Egg-based vaccines:
an A/Victoria/4897/2022 (H1N1)pdm09-like virus; (Updated)
an A/Darwin/9/2021 (H3N2)-like virus;
a B/Austria/1359417/2021 (B/Victoria lineage)-like virus; and
a B/Phuket/3073/2013 (B/Yamagata lineage)-like virus.
Cell- or recombinant-based vaccines (for those allergic to eggs)
an A/Wisconsin/67/2022 (H1N1)pdm09-like virus; (Updated)
an A/Darwin/6/2021 (H3N2)-like virus;
a B/Austria/1359417/2021 (B/Victoria lineage)-like virus; and
a B/Phuket/3073/2013 (B/Yamagata lineage)-like virus.
Info about the RSV vaccine.
RSV vaccines are recommended for those between 32-36 weeks pregnant, over 75 years, and those over 60 years with these predisposing conditions: Chronic heart or lung disease, weakened immune systems, diabetes, obesity, living in a nursing home or long-term care facility.
The RSV vaccine protection lasts several years. If you have received a RSV vaccine in the past, you do not need to get another one at this time.
These are the RSV vaccines available and the CDC does not recommend one over the other.
Arexvy (GlaxoSmithKline) is a single dose, recombinant protein vaccine.
mResvia (Moderna) is a single dose, mRNA based vaccine.
Abrysvo (Pfizer) is a single dose, protein based vaccine. This one is recommended for those over 60, or those between 32 and 36 weeks pregnant.
Vaccine hesitancy is up across the board in America, mostly due to vaccine misinformation and disinformation on the internet. Vaccines are one of the most important and impactful ways to prevent infection with bacteria and viruses. While some people have pre-disposing conditions that prevent safe vaccination, vaccines are safe and effective for most people. Discuss your vaccine strategy with your physician. Don’t get your medical information from randos on social media. Get your vaccine information from experts and physicians.
Stay happy, healthy and informed,
Jessica (an actual vaccine expert) at TCA.
The National Respiratory and EntStaying Up to Date with COVID-19 Vaccineseric Virus Surveillance System. CDC.
Staying Up to Date with COVID-19 Vaccines. CDC. September, 2024.
COVID-19 Vaccines for 2024-2025. US FDA. August, 2024.
Comirnaty product insert. Pfizer.
Spikevax product insert. Moderna.
Novavax product insert. Novavax.
Information for the 2023-2024 Flu Season. CDC.
COVID-19 Care for Uninsured Individuals. US Dept. of Health and Human Services.
RSV Vaccines for Older Adults. CDC.