TCA, vol 16. Do masks work? Part 3.
Some work better than others. In certain situations. With certain viruses.

The holiday season is upon us, and many of us will be traveling to parties and family dinners. Whenever people travel, especially during the holidays, there is usually an uptick of infectious disease, and we have seen a modest increase in COVID-19 rates following the Thanksgiving holiday. ~42,000 cases were reported per week on Nov 21, and increasing to ~56,000 per week on December 5th. Now that we are gearing up for December holiday travel, the CDC is again recommending that we mask up to prevent spreading COVID and other respiratory pathogens like Influenza and RSV.
But do masks work? I’ve been looking through the literature over the past few weeks and the data is in disarray. There are many types of studies, like observational studies (which are frought with counfounding variables, covered in TCA vol 13), there are mathematical modeling studies (which only predict best-case scenarios, covered in TCA vol 14), there are laboratory mask testing studies (covered here) and there are randomized controlled trials (which are the gold standard of clinical trials, covered in a future issue of TCA). Depending on the study, mask effectiveness varies from none at all, to modest, to great. Not helpful.
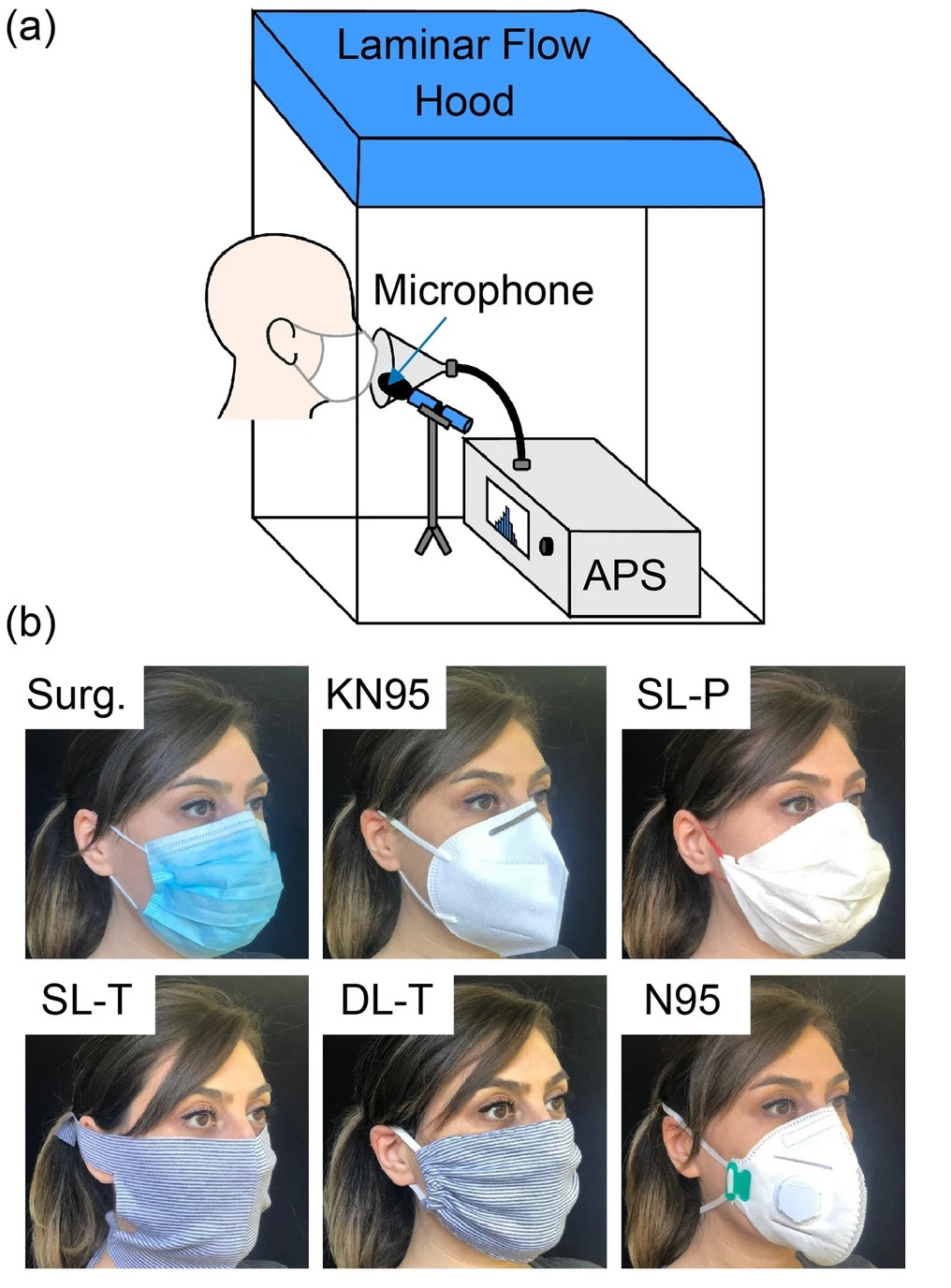
In this particular study from Nature Medicine, people wearing different types of masks were put into a chamber in front of a collector and asked to breathe, speak, cough and move their jaw around (as if they were chewing gum). The collector counted the number and size of the particles that made it through the mask. Important note: the collector did NOT necessarily collect particles that came out of the top, bottom or sides of the mask, so this is a limitation which may not reproduce real-world mask settings.
They studied 6 different types of masks: Surgical, KN95, a homemade single layer paper towel mask (SL-P), homemade T-shirt masks that were made using a CDC tutorial (single layer: SL-T, double layer: DL-T), and a N95. Just a heads up, the only difference between a KN95 and an N95 is that one is certified in China (KN95) and the other is certified in America (N95). They only had two participants wear N95s, and that’s not really enough to do any meaningful statistics, so I’ll just omit that data from my analysis (but they were pretty much the same as KN95, as expected).
So here we see the number of particles expelled into the collector when breathing (panel a), talking (panel b), coughing (panel c) and moving your jaw (panel d). Each colored dot represents a single person. Here are the takeaways:
Surgical masks did the best job at reducing expelled particles in all situations (for example, a six-fold decrease in particles while breathing and 10-fold decrease during talking).
KN95s also reduced particles, did as well as surgical masks when breathing, but slightly less well in all other scenarios.
DIY paper masks did as well as surgical and KN95s when breathing, but then did much worse under the other scenarios and was basically the same as no mask for coughing.
Double layer T shirt masks were the same as no mask for breathing and talking, and actually INCREASED the number of expelled particles for coughing and jaw movement (*see note below).
Single layer T shirt masks were the worst. They actually INCREASED the number of expelled particles in each scenario, compared to no mask (*see note below).
*NOTE: They found in a different experiment where people were rubbing the T shirt masks between their fingers that these masks released a lot of fabric fibers. These small pieces of fabric were also detected by the machine as “particles”, so its impossible to tell if the increase in particles seen in the colorful dotty chart above was due to the T shirt mask allowing the person’s respiratory droplets through, or if they were fabric particles. The authors conclude that they cannot accurately determine the effectiveness of the T shirt masks because of that.
Another interesting finding of this study is that wearing masks changed the size of particles expelled compared to no mask (it is thought that smaller particles may linger longer in the air and breathed in more readily).
Surgical and KN95s reduced small particles by up to 92% while breathing, talking and coughing.
The paper mask reduced small particles by 60% for talking and breathing, but INCREASED them by 77% for coughing
Both types of T shirt masks increased small particles compared to no mask. Single layer T shirt increased small particles 600% for talking, and double layer T shirt increased 300% for coughing (*see note above)
For the figure below, the color dots under the horizontal black line indicates a reduction in particles for that size, any color dots above the black line indicates an increase in particles for that size.
The takeaway for this study: Surgical masks and KN95s were the best at reducing all types of expelled particles, in all scenarios (for example reducing particles by 90% and 74% for speaking and coughing, respectively). Surgical masks performed a little better, but that may be because they were not performing “fit tests” for KN95s to make sure they were fitting properly (you really should be getting a fitting for KN95s since it affects how well they work). They could not accurately determine the effectiveness of DIY paper or T shirt masks because they released a lot of fabric particles (do those particles carry viruses? No one knows).
Another study in Nature looking at actual respiratory disease uses a machine called, I kid you not, the Gesundheit-II. In this experiment, participants infected with either coronavirus (not the type that causes COVID-19 though), influenza or the common cold breathed into the Gesundheit-II machine either wearing a surgical mask or not. They then tested the particles for the presence of actual viruses.

For coronavirus: masking reduced the detection of viruses in large particles from 3/10 (no mask) to 0/10 (mask) although this was not statistically significant. Masking reduced viruses found in small particles from 4/10 (no mask) to 0/10 (mask).
For influenza: masking reduced the detection of viruses in large particles from 6/23 (no mask) to 1/25 (mask). Masking reduced viruses found in small particles from 8/23 (no mask) to 6/27 (mask), although this was not statistically significant.
For the common cold: masking reduced the detection of viruses in large particles from 9/32 (no mask) to 6/27 (mask) although this was not statistically significant. Masking reduced viruses found in small particles from 19/34 (no mask) to 12/32 (mask), although this again was not statistically significant.
The takeaway: Surgical masks reduced the presence of coronavirus in small exhaled particles and influenza virus in large exhaled particles. The masks also reduced all viruses in all other scenarios but not in a statistically significant way.
The HotTake: Certain masks can reduce expulsion of some particles, and some viruses, and during some activities.
But not all masks (paper towel and T shirt, maybe) and not all viruses (common cold) and not all sized particles. So, again, this kind of explains why there is so much variation in observational studies… because the results vary based on the scenario. Plus, the lab experiments above are done under very controlled temperature and humidity conditions: both of which have been shown to influence the spread of respiratory disease. So, this does not accurately represent real-world scenarios which would be under varying temperature and humidity, different people wearing different types of masks, etc.
Results may vary.
Respiratory Virus Shedding in Exhaled Breath and Efficacy of Facemasks
Stay happy, healthy and informed,
Jessica at TCA